DOWNLOADS
path: COT RESOURCES
- old documents
- confidentiality.pdf
- cot – blank marking sheet – rcgp.docx
- cot – criteria in detail – rcgp.docx
- cot consent form.pdf
- cot consent process.doc
- cot mapping.doc
- cot on 2 sides of A4 for trainers.doc
- ethical guidelines for recording patients on video.doc
- intro to cot by yh deanery.pptx
- video allergy – overcoming it (TEACHING RESOURCE).doc
- video consultation analysis – csa style.doc
- writing COT feedback template for 14Fish.docx
What is the COT & what's it testing?
The COT is primarily about consultation skills. And consultation skills are not just about communication skills – there’s skills like ‘making a diagnosis’, ‘formulating a reasonable management plan’ and so on.
The only way you’re going to become good at this skills is if you repeatedly practise them. That’s the key! Remember riding a bike for the first time? At first you couldn’t do it. Then, after a while, you could but you kept swaying and falling off. Finally, with more practise, you could do it no problem. And finally, after further practise, you became a master at it and could do all sorts of things like wheelies and jumps. The same goes for all these consultation skills – practice makes perfect.
And once you become really good at consultation skills…
- Watch how the accuracy of your data gathering (and thus diagnoses and management plans) improve significantly
- Watch how you manage to do things effortlessly in less time!
- Watch how you are able to manage difficult situations and resolve them
- Watch how your patients really like you and think you’re a great doctor because you develop a management plan that is tailored to their needs and priorities (yet balanced against what you as the doctor thinks is necessary or not).
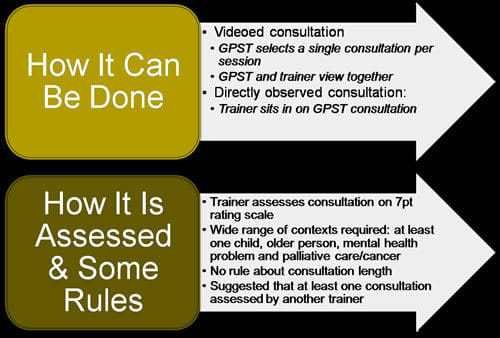
How does COT work? Explain the process.
- Your timetable should have one surgery per week marked as a video surgery. Each slot will be about 20 minutes long. The practice should have a system for informing patients that this is a video surgery, and getting consent from them before AND after the surgery. Check with your Practice Manager that this is all in place.
- During that surgery, make sure you just switch the video camera on. Your practice will have provided you with one.
- Then, before the video COT tutorial with your trainer, have a look at the videos you have recorded and determine which one or two you would like the trainer to observe and assess.
- Then on the day of the tutorial, you and your trainer will sit down and watch the video. The way the trainer does this may vary from session to session. Sometimes the trainer might watch it all the way through. Other times, the trainer might stop the video intermittently and discuss/highlight various points. The trainer will be marking the COT sheet as the video is being watch and they may even get you to mark it too – so they can gauge whether you’re both on the same thinking track.
- And of course, at the end (or sometimes during), there will be feedback, recommendations for further development and agreed action which should help you with future ones. Remember, the focus is on progressive development.
- All of this will then be documented in the electronic COT assessment form in your ePortfolio.
Quick Note to Trainers:
When filling in a COT assessment sheet electronically, please add a brief description of each COT in the electronic RCGP COT form under the heading “Title of Procedure”. It might look as if there’s no room to write much, but if you start writing the space will expand for you to write more. Something like ‘32y old woman with abdo pain, distressed, poor English’ – enough for the ARCP panel to know what the consultation was about.
Which sort of video cases should I select? And advice?
As with CbD, COT case selection is important as different cases will demonstrate different consultation performance criteria. Please do not pick simple easy consultations because they aren’t very good at demonstrating what you are good at.
For example, let’s say I’m a relatively newly qualified driver. And I would like to take you on a trip to Birmingham. Which of the following scenarios would reassure you the most that I am hopefully a very safe and competent driver?
- Scenario 1: I offer to drive you around the block. The journey is straight forward and it will be over in 5 minutes.
- Scenario 2: I offer to drive you at night time at about 1 am. I’ll drive for about 5 miles in the country side. The journey will be about 30 minutes.
- Scenario 3: I will drive you to the next local town which is about 5 miles away. The journey will be about 30 minutes. We will go during the day because that’s the time we will hopefully set off to Birmingham, if you agree.
I hope you have chosen Scenario 3 as the one that would reassure you the most out of these 3 options. Scenario 1 – is TOO SIMPLE and EASY. But it provides very little assurance that you can drive well. You will only be driving for 5 minutes and the trip to Birmingham is 2 hours! Scenario 2 is also TOO SIMPLE and EASY. It’s country lanes and you’re travelling at a time when no cars will be about! And don’t forget, the trip to Birmingham is going to be motorway so it provides no assurance over the driver’s handling of that. But scenario 3, whilst not 100% reassuring, is better than the other two. You will be driving to the next town, on the motorway, for a good length of time and at a time when other cars will be about and so being able to drive amongst that lot should provide a much better level of reassurance.
What’s the point of telling you all of this?
If you pick simple easy peasy cases, you will not demonstrate with enough depth the various criteria on the COT performance marking crib. So, my advice would be to pick challenging difficult consultations. For instance,
- pick consultations that were complex – medically complex or psychologically complex or socially complex or ethically complex!
- pick consultations which you think did not go well in terms of the doctor-patient interaction. Perhaps the patient got angry, was demanding, walked out or did not agree with your management plan. These sorts of scenarios push you to your limits and in so doing, will help bring out behaviour within you that is assessable and many will at a competent level. Trust me – take a chance – try it and see.
Finally, if you pick challenging consultations like these, believe me – you will educationally get more out of them as your trainer helps your find alternative ways of handling things better.
I manage to record 5-6 consultations but in a tutorial we only look at 1 or 2...
Okay, you may feel a bit dispirited that you went to all the effort of recording 5 consultations and the trainer, in the tutorial looked at only ONE of them. Your feeling is understandable. But please don’t be dispirited! If your trainer has selected the one consultation, that’s because they want to look at in detail and help you perform even better the next time around. Which would you prefer: A trainer who goes through 4-5 videos per session and just skims through them, marks you, talks a bit about them OR the trainer that looks at 1 or 2 and really digs deep and through conversations with you, truly understands your strengths and difficulties and is able to help you with those difficulties so that you may perform better in the future?
We understand that you want to do as many COTs as possible because it looks good on your ePortfolio. But surely, it is better to look at less and do them in a more deep and meaningful way. And of course, if you only looked at ONE COT per week, after 4 months of training, you would have 16 COTs! There is plenty of time to get the numbers in if you plan well. Remember, you will never get a trainer again after your GP training period is over – so make good use of them while you can.
A little word of warning about using scripts and phrases
Generally, we don’t recommend memorising scripts and phrases because a conversation between two people naturally flows when they respond to what each other has just said. Scripts and phrases can make the consultation look artificial or contrived. However, we’ve provided them here because we know that many trainees would like an ‘idea’ of the kinds of things to say as a starting point. Please develop your own phrases and remember to contextualise them according to the specific situation you are in as you become well versed in them. Then, things will start to look really natural. (And they’ll love you in the CSA).
A big word about the video camera
Please remember that the video camera must be carefully guarded. It is your responsibility to keep it safe. DO NOT LEAVE YOUR CONSULTING ROOM FOR LONG PERIODS as the camera might get stolen. The problem with the camera getting stolen IS NOT the cost of replacement (most are relatively inexpensive these days anyway). The problem is the BREACH OF CONFIDENTIAL PATIENT DATA. And for that, the practice can be sued for THOUSANDS OF POUNDS. So, please guard the camera for the entire period of your post. Never leave it unattended. Never leave it in an unlocked drawer. Never leave it lying around in your pigeon hole. Get into the habit of deleting OLD videos (to minimise the amount of patient recorded data on there). And at the end of the post, wipe all patient videos from it before handing it back to your Practice Manager.
I really hate being video'd
LOts of people hate being video’d – not only trainees! I know many trainers – who are reapproved every 5 years and have to bring videos to show how they teach things like COTs and CBDs – also hate doing the video thing! You are not alone. And it is okay to feel like that. It can be very unnerving having someone look at your videos and assess you.
I would like to ask you one question though. Why is it you feel like that?
- If it is because you are worried about showing your deficiencies and do not want to look bad – again, that is understandable. However, it is also worth remembering that we trainers know that you as trainees have lots to learn and each of you will have a different starting point. We tend not to think how good or bad you are but instead we try to think where you are in your training journey and how we can best train you and move you to a higher level.
- If it is because you don’t like some of your behaviour or actions, then what better place to improve on them through video. Would you rather not pick up on what you would like to change and not work on it? The video is a massive opportunity to look at yourself with your own eyes (and of course, that of the trainer’s) and work together to improve bits and bobs until you get to a point where you are no longer uncomfortable with the things you once used to do!
- If it is because you simply don’t like seeing yourself, or your “squeaky” voice, again don’t worry. Yes, you will notice small things about yourself that you may not like on video. It’s important to remember that these things ARE SMALL and it’s highly likely that your trainer won’t even notice them – you’re awareness to these micro-signals are usually heightened and out of proportion. But your trainer hears and sees you every day and thus will not find your voice particularly ‘squeaky’ or your hair looking bad! In fact, they will be focused on your behaviour, your actions, the way you interact with the patient and the way the patient interacts with you. And another thing – the more you video, the more you get use to seeing and hearing yourself on video and eventually you will not give a hoot! Things will get better the more you do video – promise!
And finally, remember who is assessing you – it’s your trainer who we hope you will see as a warm friendly person who only has YOUR best interest at heart. They want to help you do even better, but they cannot do that with COTs if you are unwilling to show yourself, take a little risk and change your mindset from one of apprehension to one of eagerness to learn.
Can I do COTs on live consultations rather than video?
Yes, yes and yes! In fact, it is STRONGLY recommended that some COTs are done on directly observed consultations, i.e. where the trainer sits in with the trainee. This will help trainees get used to consulting with someone watching (especially good for CSA). Also, it means that a range of normal consultations are observed by the trainer, not just the good ones which trainees tend to select for COTs. And it’s another way of seeing exactly what happens in real life.
The trainee hates doing video. Can all COTs be directly observed in consultations?
In short – NO! COTs were initially designed to be done on video consultations. So – this STILL NEEDS TO HAPPEN. Yes, you can do some on directly observed consultations (which we’ve said is good practice) but not totally at the expense of doing no consultation videos at all. Why? Because both methods have pros and cons. And actually, if you had to choose one, videos has the edge on live consultations. But what is best is if you can do a mixture of both (with predominantly more video). Have a read of the pros and cons and see for yourself.
DIRECTLY OBSERVED LIVE CONSULTATIONS
Pros
- It is a real-life consultation on the go. Some argue that this is a real and live demonstration of performance . (But read the comments below)
Cons
- The Hawthorne Effect: Many trainees get flustered when someone watching them. Hence the trainee is prone to making blunders with the trainer sitting in. Or conversely, some trainees can put on a super performance only for when the trainer is there but don’t do it routinely in their work. In Summary, the Hawthorne effect is when you do or don’t do things that you would or would not ordinarily do, but you do so for the simple fact you are being watched. It is more likely with a person sitting in than with an inaminate object like a video.
- The trainee cannot see him or herself. It is impossible for them to step outside of their body and observe themselves. Therefore, it is difficult to reflect. If it is difficult to reflect, then it is difficult to learn and improve one’s performance.
VIDEOS
Pros
- The trainee can see themselves and observe what they do and don’t do. This is more powerful and transformative in terms of learning than someone just telling them. A trainee is more likely to change their behaviour if they can SEE for THEMSELVES what they do and do not like.
- And you can rewind a video to show them exact points you want to talk about.
- The Hawthorne effect: is less likely with an inanimate object like a video sitting in the corner – which is soon forgotten after a couple of patients.
Cons
- The trainee can cherry pick consultations and show you what they can do, but not necessarily what they actually do in every day performance.
Examples of good and bad COTs

