Teaching & Learning
The PDP
DOWNLOADS
path: PDPs
What is a PDP?
The PDP is short for Personal Development Plan. It is an educational tool (within the ePortfolio) to help the trainee’s document their learning and development needs (and wants) over the following 6-12 months.
A good personal development plan (PDP) will set out how a trainee assessed their learning needs, how they plan to address these needs and the evidence they will provide to demonstrate their learning. The whole point of the PDP is to help you focus on what it is that you want to achieve and by defining this, you end up with a navigation tool that will direct you over the next 6 month post.
Why do I need a PDP if I have identified my learning needs elsewhere?
You’re right, learning logs for example, also help you identify learning needs to help you become a better doctor. So why have a PDP? Well, most of a doctor’s learning occurs continually in the workplace and this is the sort of stuff that you should be recording as learning logs. However, the PDP should NOT be thought of as a learning log, but as a TOOL, for prioritising and tackling some of the bigger stuff. So, amongst all the learning needs you identify from learning logs (and other places), some you can do easily, but others require a bit more care and thought – because they are either more complex or weightier. And it’s the PDP that helps you focus on what are those bigger things that you would like to focus on the next 6 months or so.
It should not be assumed that learning derived from a PDP is some way superior to that which occurs in learning logs or other naturally adhoc ways. By now, you should realise that the two approaches are complementary. So, in summary, PDPs are a collection of learning things that you want to do driven by events recognised during practice and usually directly concerning patient care.
For example, you might realise from a learning log that in terms of Future Development Needs, that you need to read and understand the GMCs guidance on consent and confidentiality. That’s not really a big task – can be done in less than an hour – and you’re done. That’s the sort of thing that you might do one evening or at a weekend.
PDPs on the other hand take longer to do and sometimes can’t be done quickly in a day. They may need several “revisits” and may need to be worked on incrementally. For example, you realise from a patient encounter (and perhaps from a learning log as a reflection after the event) that you’re really not very good at contraception and HRT. So, you’ve not only booked onto a Women’s Health course but also decided to read about it and sit in with Dr Sarah, who is the lead in the practice for Women’s Health. Can you see how chunkier that is than the former?
The ARCP panel will expect to see entries at least every 6 months to demonstrate engagement in learning and reflective practice (Competency area 10).
What types of things serve as PDPs?
Learning can only ever be one of three things – Knowledge, Skills or Attitudes (KSA for short). So, it in the example about, if I want to learn more about Women’s Health and I intend on reading and going on a course – then that is a KNOWLEDGE thing. If I want to go on a practical course on dermoscopy or advanced communication skills, then that will be a SKILLS thing. And if I went to a discussion group about asylum seekers and refugees and it changed your view of them, then that would be an ATTITUDINAL thing.
PDP cycles can be about a Knowledge thing, a Skills thing or an Attitude thing.
Can you give me an example?
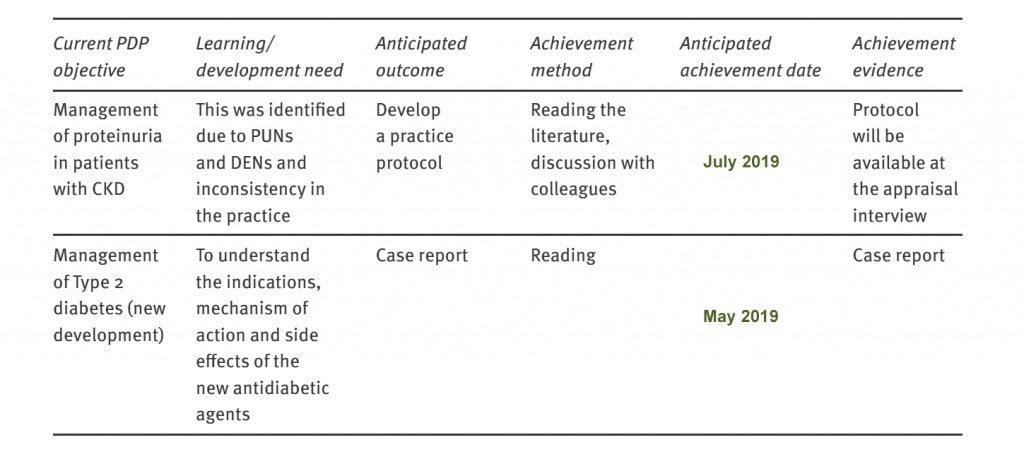
Learning can only ever be one of three things – Knowledge, Skills or Attitudes (KSA for short). So, it in the example about, if I want to learn more about Women’s Health and I intend on reading and going on a course – then that is a KNOWLEDGE thing. If I want to go on a practical course on dermoscopy or advanced communication skills, then that will be a SKILLS thing. And if I went to a discussion group about asylum seekers and refugees and it changed your view of them, then that would be an ATTITUDINAL thing. Take a look at the example below.
Bad and Good Examples
WHAT
To keep up to date with new clinical developments
HOW
Attend tutorials
WHEN
Over next 6-12 months
OUTCOME
Pass exams and assessment
Learn about gynaecology as applied to general practice
Attend tutorials and ward rounds during ST2 job in O&G
Over next 6 months
Be more confident
Become more proficient, thorough and confident in taking sexual health histories
Practice within joint consultations
During GU attachments during O&G job
Improve proficiency as shown through a relevant CBD and mini-CEX
Which of these are good and which are bad?
Answers:
The first one is not SMART, as the objective is broad and general. There is no measurable or specific endpoint – when does a doctor finish keeping up to date? The second one is not SMART for the same reasons as above. The third one is good – the need for this objective was identified during a clinical encounter and recorded in the shared log. So the answer is – The 3rd is good, but 1 and 2 are bad.
A database of PDP actions
We know both trainees, trainers and Educational Supervisors often find writing PDPs difficult. That’s understandable because it is not an activity that you do every day, like examining patients! So, here is a database of examples to help you. They are grouped under the RCGP’s Professional Competency headings because that is what the trainee is ultimately assessed against BUT ALSO because your are writing your PDPs to provide evidence for learning in these competency areas.
How to structure your PDP (SMARTIES)
- The educational need is identified through natural activities at work.
The need and how it arose should be clearly stated – either referenced to a log entry or directly inserted into the PDP.
The learner can show how the needs identified reflect the needs of patients, practice/employment setting, and the expectations of the GMC, as well as their own interests. Some of this will relate to the needs of the practice, patient views, and key areas of GMP or other GMC documents. - Aims are converted to learning objectives.
Clarification of objectives in relation to each need is necessary to help break it down and work on it. Use SMARTIES as detailed above. When writing your objectives ensure that they are specific and, in your view, achievable. Measurement of objectives should only be encouraged where this appropriate. - The activities proposed for addressing the learning needs are stated.
Start by identifying the first steps that you need to take in order to address your development need. Your Trainer/ES should be able to help you if you get stuck. - The reasons for any changes made to the development plan are stated
Any changes, particularly deletions, should be justified. - There is appropriate evidence to demonstrate learning.
- This should be stated and should be relevant to the development objective(s)
- There should be some reflection on the learning
- Reflection on learning can be facilitated through discussion with the Trainer/ES.
This easy to remember mnemonic will help you structure your PDP and make it not only easier to write about but also easier to achieve.
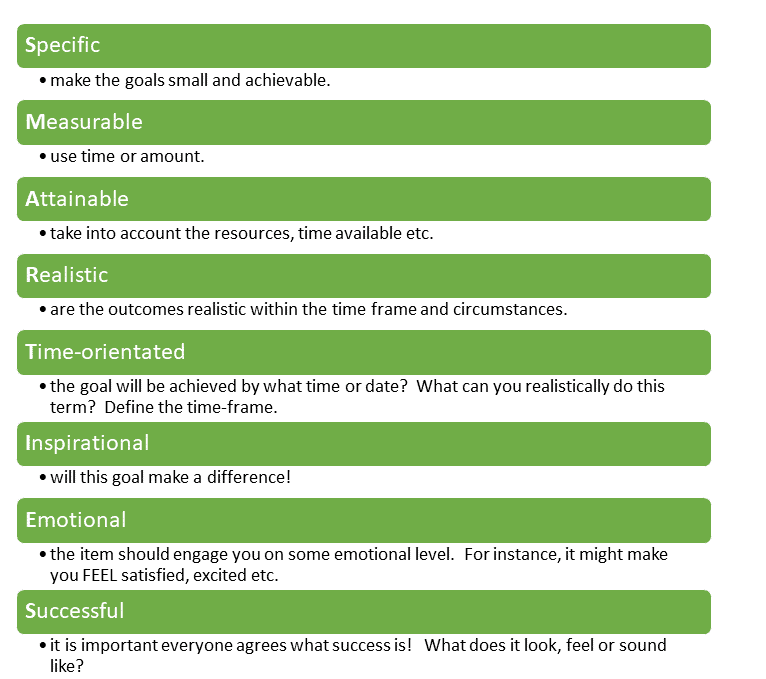

- Specific: they should relate to specific tasks/activities, not general statements.
-
- BAD: “I want to improve my consultation skills”
- BETTER: “I want to learn some Motivational Interviewing techniques” or “I want to learn techniques to diffuse the angry situation”
-
- Measurable: it should be possible to assess whether they have achieved.
-
- BAD: “I will show improvement through my daily consultations”
- BETTER “I will have attended a course and will write up some reflections. I will also document 3 consultations where I have used these new techniques”
-
- Achievable: it should be possible for the doctor to achieve the desired outcome.
-
- BAD: “I want to learn everything about Women’s Health because it is a weak area of mine”
- BETTER “I want to improve my knowledge in common Women’s Health areas – namely menstruation difficulties, contraception and the menopause”
-
- Relevant: objectives should be appropriate for the current role and situation.
-
- BAD: “I want to improve my knowledge of rare neurological disorders” (Why if you’re not going to be a neurologist?”
- BETTER: “I want to improve my knowledge of MS and the services available” (Because MS is not uncommon in General Practice)
-
- Time-bound: there should be a clear time frame set in which to achieve objectives.
-
- BAD: “I will do this soon”
- BETTER: “I will do this before September 2020” or “I have found a Motivational Interviewing course schedule for Sept 2020 in Birmingham and will attend that and write up reflections aafterwards.
-
Any final top tips?
- PDPs should be broad statements of what you want to achieve during the current post. Things like
- I want to be better at communication skills – especially explaining things to patients
- See loads of skin conditions to improve my clinical knowledge of Dermatology
- PDPs should reflect your learning needs. Learning needs can only be one or more of Knowledge, Skills or Attitudes. Therefore, try and define you PDP item explicitly by defining what knowledge, skill or attitude you are trying to build on.
- Remember, you can directly formulate a PDP from a learning log by hitting the “Send to PDP” button – this saves you writing it out all again.
- Do not put things like passing the AKT or CSA or write more log entries as your PDP – because these are routine things that are expected of you anyway!
- To add structure to your PDP item remember the mnemonic SMARTIES: PDP items should be Specific, Measurable, Attainable, Realistic, Time Framed, Inspirational, Emotional, Successful. Add further structure by numbering or bulleting the list of actions you need to take.
- And if you don’t have time to write out the PDP item completely, why not just add something ‘quick, rough and ready’ for the time being to serve as a signpost for you to smarten up later?
- Your PDP may change throughout the course of your post as new and more important learning gaps and needs are identified. It is completely okay to change your PDP and prioritise things. PDPs are meant to be alive and dynamic – changing with the external environment and its demands.
- And finally, you don’t have to fill in every box of the eportfolio’s PDP page; it’s only there to guide you – some find it helpful but others find it too restrictive. The box most people struggle with is “How will I know when it is achieved”. If this is too difficult for you to fill in, don’t worry. As long as you’ve written up your reflections, learning points and future learning, that should be enough.
- Put in a couple of diary date reminders to look at your PDP to ensure you are working on them in a timely way. This will help avoid last minute chaos and action. Don’t forget to update your PDP and show what you have done about it before your ES meeting.
FAQs
Somewhere between 3 and 5.
There is no “pass mark”, but where several standards are not achieved and Educational Supervisors will consider a PDP to be unsatisfactory.
- Learning areas to be put in the PDP will arise continuously during day-to-day practice and should be documented in the learning log. Entries can be transferred to the PDP (by clicking Send to PDP) when log entries identify learning needs and a plan how to address them has been entered.
- The Clinical Supervisor, may assist to identify those that are most important, so that they can be prioritised and, if necessary, allocated resources in terms of tutorial time, study time or study leave.
- It is also an important part of the Educational Supervisor review to review the PDP, discuss progress and help plan the main learning areas for the forthcoming 6 months
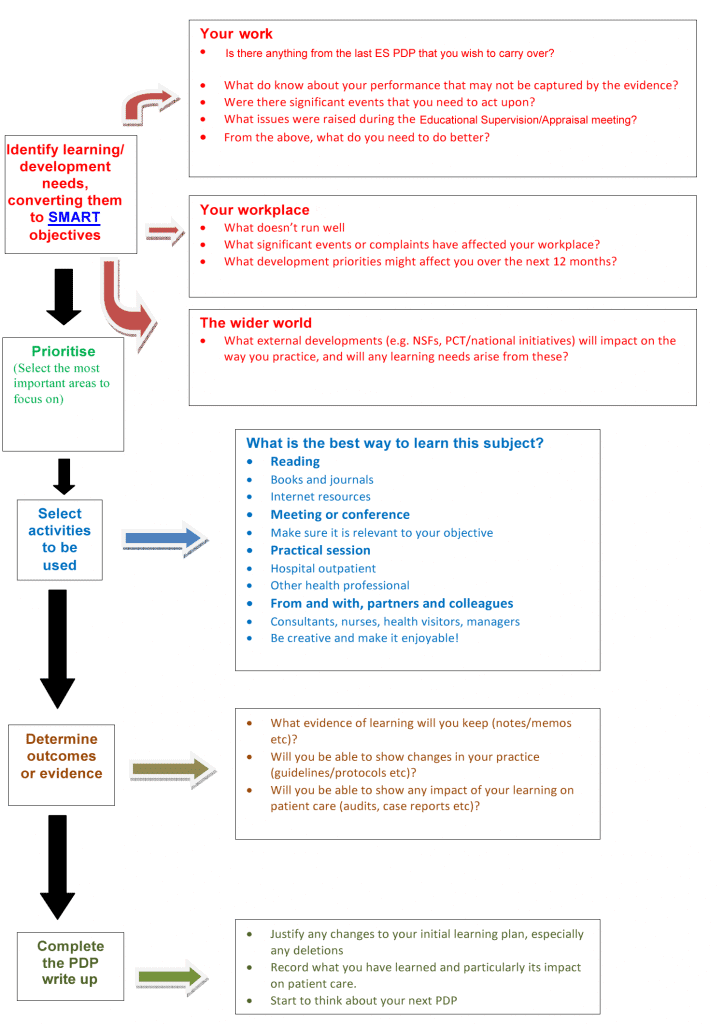
And finally
A great little infographic from Amar Rughani & Nick Field. I think this summarises everything nicely.



Thank you for this comprehensive information on PDPs.